Is it the beginning of the end for dubious American clinics that sell transplants of unproven and non-FDA approved fat stem cell injections?
As the year of 2014 was winding down, the FDA issued two key new draft guidances (see here and here) that could prove to be crash diets for these burgeoning fat stem cell clinics. (Update: As of 2020, the FDA has now clearly defined fat stem cells as drug products and filed suit against two firms marketing unapproved fat stem cells.)
These new FDA guidances indicate that the stem cell products used by scores of dubious stem cell clinics in the US are almost certainly drugs for which pre-marketing approval and licensing (biological license application or BLA) from the FDA are required in advance of use on patients.
The clinics don’t have that licensing or approval, but they are transplanting stem cells into thousands of patients a year any way and making millions doing it.
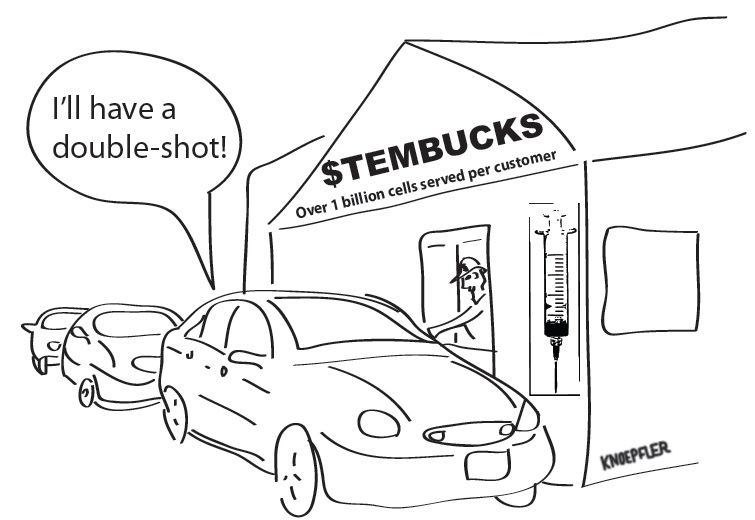
In 2012 I imagined in a cartoon (below) a possible future if the stem cell clinics got their way for extreme deregulation. These new 2014 draft guidances are a strong signal that appropriate regulation of the stem cell clinic industry is not going away.
In fact, these new FDA guidances more squarely put scores of such dubious stem cell clinics in the US on a regulatory collision course with the agency.
Could the clinics win out in such a conflict?
It’s very unlikely.
The regulatory path may be a slow one and these are so far just draft guidances, but the eventual outcome is not in much doubt. It is not a question of if, but rather when.
These clinics and their doctors cannot continue with their status quo of using patients as guinea pigs for profit now without serious legal risks to themselves. Indeed, the one thing that could alter the impending collision is if the clinics change course and mend their ways to be compliant in a regulatory sense. It’s hard to imagine that happening, but it is possible that some will try. I hope so.
I suppose the clinics could also try to sue the FDA, but that would likely be a huge waste of money as the FDA would almost certainly prevail in court given legal precedent.

The newer of the two FDA guidances that came out at the end of the past year is specifically all about fat (or adipose) stem cells.
Fat stem cells are the stem cell product of choice for most dubious clinics in the US today. Their fat stem cell product is most often called “stromal vascular fraction” or SVF, which is made by enzymatically liquefying the fat tissue and spinning it through a column to isolate just the cellular “stem cell” part of the fat.
You can see a diagram that I drew of the method to make SVF from my book on stem cells. It’s hard to imagine the stem cell clinic argument that the SVF (cell pellet at the bottom of that tube) is the same thing as the starting fat tissue.
The new FDA guidance makes it crystal clear that regardless of other circumstances, if a clinic makes SVF it is a biological drug legally requiring pre-market approval and licensing by the FDA before you use it on patients.
Again, to my knowledge 100% of these clinics do not have such FDA approval.
The top rationales put forth by the clinics for why they do not need FDA approval seem even more outlandish today after these new guidances.
For example, clinics often claim that the fact that they transplant the fat stem cells in a “same day” surgical procedure makes the fat stem cells not qualify as drugs. The new guidance says that reasoning is invalid if the product is more than minimally manipulated and to be clear it says that fat stem cells are more than minimally manipulated.
Another important issue is non-homologous use of fat stem cells. The clinics often sell fat stem cell transplants to supposedly help a surprisingly wide array of conditions that generally have nothing in common with fat. For example, the clinics sell fat stem cells to treat neurologic or orthopedic conditions or for sexual dysfunction. The FDA draft guidance says that such non-homologous use automatically means that the fat stem cells are drugs regardless of other circumstances.
There is a compelling logic to the FDA guidance here. Fat is fat. It is not nerve or cartilage or other kinds of tissues. This doesn’t mean that fat stem cells cannot ever be used to treat other kinds of conditions, but rather it just means that there is an appropriately rigorous requirement for scientific data in advance before such use should occur.
What should the fat stem clinics do now? Given these new guidances, if I were such a stem cell clinic doctor, I would be stopping my clinic operations right away at this point so as to avoid serious legal ramifications. Otherwise there is a good chance in the future that you will receive a visit from the FDA, perhaps a warning letter, and they may shut you down. Such FDA action may also be a sound legal basis for patients to sue you for malpractice as well.
Below are some key quotes from the newest FDA guidances, which could give the clinics operators some sleepless nights because they sure seem to directly indicate that what the clinics are doing is making and using unapproved biological drugs, which is almost certainly contrary to FDA regulations and hence the law (emphasis mine):
“Example A-1: Adipose tissue is recovered by tumescent liposuction. The adipose tissue undergoes processing or manipulation (e.g., enzymatic digestion, mechanical disruption, etc.) to isolate cellular components, commonly referred to as stromal vascular fraction, which is considered a potential source of adipose-derived stromal/stem cells for clinical therapeutic uses. This processing breaks down and eliminates the structural components that function to provide cushioning and support, thereby altering the original relevant characteristics of the HCT/P relating to its utility for reconstruction, repair, or replacement. Therefore, based on the definition of minimal manipulation for structural tissue, this processing would generally be considered more than minimal manipulation.”
“Example B-2: Adipose tissue is recovered and processed for use, as reflected by the labeling, advertising, or other indications of the manufacturer’s objective intent, to treat bone and joint disease. Because adipose tissue does not perform this function in the donor, using HCT/Ps from adipose tissue to treat bone and joint disease is generally considered a non-homologous use.”
“Example A-2: Adipose tissue is recovered by tumescent liposuction. Stem cells from the lipoaspirate are then isolated. Cell isolation would typically cause the adipose tissue to no longer be “such HCT/P.” Thus, even if this processed HCT/P from adipose tissue is injected into the same patient from whom it was removed during the same surgical procedure, the establishment would generally not be considered to qualify for the exception under 21 CFR 1271.15(b).”
In order to lawfully market a biological product, a biologics license must be in effect (42 USC 262(a)). Such licenses are issued only after a determination by FDA that the establishment(s) and the biological products meet the applicable requirements to ensure the continued safety, purity, and potency of such products (21 CFR 601.2(d)).
In the end, this new FDA guidance is appropriate and when finalized will further protect the public from dubious stem cell clinics that today are making big bucks off of vulnerable patients via unapproved as well as potentially harmful and ineffective stem cell “treatments”.
Some helpful background posts and FDA links:
- https://www.ipscell.com/2013/03/you-want-sauerkraut-on-those-stem-cells-defining-the-term-unlicensed-stem-cell-clinic/
- http://www.fda.gov/BiologicsBloodVaccines/DevelopmentApprovalProcess/BiologicsLicenseApplicationsBLAProcess/default.htm
- https://www.ipscell.com/2014/12/breaking-new-fda-draft-guidance-views-fat-stem-cells-as-drugs/
- http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/CellularandGeneTherapy/ucm427692.htm
- http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Tissue/ucm419911.htm
- https://www.ipscell.com/2014/12/new-interview-with-fda-on-key-stem-cell-regulatory-issues-its-own-research/
Since the FDA is going to crack down on unproven treatments, the clinics will have two choices: go for FDA approval, which will be far more expensive than anything they have considered so far–or move the “therapies” to other countries, which almost certainly will increase profit margins. What do you think will happen?
Mexico, Caymans, Asia…we’ve seen clinics bolt to all of these rather than work to become FDA compliant…
How did you arrive at the conclusion that these clinics are making big bucks? Do you have access to financials? I am never clear as to where you get your information. If you would name your sources, it would enhance the credibility of your statements.
Well, we do know that they charge on average $20-$30k per treatment per patient, not including accommodation or travel (Lau et al., Cell Stem Cell 2008), and that some patients go for multiple treatments. What are their costs? They are typically not culturing the cells or freezing/storing them, so consumables costs should be low. The procedures do not require general anesthesia or rely on specialized equipment, and they are typically not sending the cells for analysis or performing cell sorting. Therefore, it seems like the overall staffing and procedural costs would be relatively low; correct me if I am wrong. Considering that for all that, they don’t have to actually show it works and basically just have to not kill the patient, it seems like it would be pretty lucrative.
I will correct you because you seem to have drawn your conclusions based on no real experience or updated information. I have no idea how you can conclude something like that from a 2008 study.This is 2015. Prices vary from clinic to clinic and also are based on the disease being treated. Stem cell treatments for COPD for instance are usually in the $5K-9K range. In 2007, the cost was $15K-$25K. That is quite a dramatic change I think you will agree. No one is forced to go for treatment. It is a choice a patient makes. For me, the results have been life changing. As more clinics open, it is also nice to be able to be treated close to home, thus saving the stress and cost of travel.
But Shinsakan, unless you are partnering with Paul on this blog, the question I asked was not directed to you because you didn’t write the article. Therefore, I would not assume you would know the source used for it, but thanks for taking a stab at it. Perhaps, he used the same source you quoted. I’d like to know.
Barbara,
Costs for other “cash cow” procedures (e.g., cosmetic surgery, dental implants) have remained relatively constant over time, so I assumed that the data of Lau et al. would still be relevant. In addition to Lau et al., I was also basing my estimate on a recent (last month) quote of $26k for an anti-cancer cell therapy for a loved one of mine. Additionally, a recent investigative report by NBC (December 2014) also found prices of $6-20,000 (http://www.nbcnews.com/news/investigations/costly-unproven-stem-cell-therapy-neurological-disorders-questioned-n262701).
Thank you for giving the current prices for COPD treatment; however, note that you are only describing prices for COPD and not the plethora of other diseases supposedly being treated. I do agree with you that $15-25k to $5-9k is quite a reduction in only 7 years. However, it makes me wonder why/how the price has been reduced so much, given that the cost to the provider likely did not similarly decrease in the same time interval. Competition among providers, perhaps? Wouldn’t their ability to absorb such a decrease suggest that at least in 2007, the clinics were making big bucks?
Regardless, I still think that even $5-9k per treatment (where patients also often come back for repeat treatments in, e.g., neurological diseases because it didn’t work the first time) would still result in a lucrative practice, especially given the apparent low cost to providers (you have not challenged my assessment of the costs or provided any reasoning why the procedure would be expensive for the provider to perform), and again especially considering that without regulation the providers do not have to show that their treatment works or even indeed to show any analysis of the cells they are transplanting. Even McDonald’s can make money off of the dollar menu by keeping costs low and not having to make any promises about the final product. I think that the “big bucks” argument still stands, and is further supported by the increasing franchising of such clinics and the fact that we now have, e.g., plastic surgeons trying to treat neurological disorders simply because of the assumption that injecting SVF will heal all diseases.
I am glad that you personally had a positive experience. My own work with MSCs/ASCs evaluated their anti-inflammatory effects, which I expect could have been involved in the therapeutic effects you observed. However, such success is not the case for everyone (or for all clinics), and appropriate dissemination of knowledge is necessary so that people can make educated decisions. Regulation is important to help improve consistency and give patients the best chances at safety and efficacy.
As for not directing your question at me, this is a blog with a comments section that is a public forum. By posting here, you invite comment from all other readers. That being said, when I was looking at it, most of the peer-reviewed literature that actually cited prices gave similar numbers to Lau et al. and was from around 2007-2009 (why I had to resort to NBC above for 2014), but I can’t speak as to Dr. Knopfler’s sources.
Shinsakan,
You make many good points. I’d also point out that in my conversation with people in one particular clinic (yes, I know this is anecdotal, but we don’t have much else to go on) that they quoted $8K per procedure for their clinic and admitted that most patients would benefit from more than one procedure to have the best chance for a positive outcome. For any kind of autoimmune disease, and let’s assume that MSCs do have significant, clinically relevant anti-inflammatory effects for the moment, it is very difficult to imagine how one treatment could lead to essentially a permanent remission as MSCs typically do not engraftment in significant numbers.
Dr. Knoeplfer,
Thanks for the comment. When I was just looking, I also found a clinic that was charging a flat fee of $7600 to use SVF to treat various maladies (one of the few websites that actually publishes prices), so the $8k figure makes sense. I am also aware of the need for multiple treatments for various disorders, especially autoimmune diseases such as MS. I also agree that for a chronic autoimmune disease, it is hard to believe that cells that mostly do not engraft after implantation would be expected to have lasting anti-inflammatory effects. I believe that the accepted approach for autoimmune diseases is initial immunoconditioning to kill off aberrant immune cells, followed by transplantation of hematopoietic stem cells that then engraft and differentiate to self-tolerant immune cells to replace the depleted aberrant cells, but this is obviously not what is being done in the SVF clinics. Some believe that MSCs exert tolerogenic effects through induction of host Tregs, but it is unclear whether or how such effects would remain after the donor cells are gone.
It’s pretty simple. I have talked to the clinic operators themselves and other doctors working with them. As you can imagine they generally do not want to go on the record though.
I can imagine that they don’t, but I have asked several doctors and clinic owners and none of them have spoken with you or corresponded in any way. A doctor working for a clinic is probably not the best source for information. Running a business can be expensive. Doctors not involved in ownership may not know the actual costs involved. I have based my comments on my own experience. The cost has come down dramatically from what I paid in 2007. COPD is probably one of the more common diseases being treated with stem cells in the U.S. along with orthopedics. Many orthopedic procedures are priced quite reasonably as well. Higher prices are more in line with neurological disease. Those cases would not make up the majority of patients being treated in the U.S. at stem cell clinics.
Barbara, I’m not sure I get your main point though. Are you saying that the clinic operators are not making any profit from doing stem cell procedures? Or that they are making some profit, but not very much? If it is the latter, what do you call “not very much profit”?
My sense is that the charge per procedure varies widely from clinic to clinic from low thousands up to above $10K and that the average patient receives at least 3 procedures. If we assume a 50% profit margin on say a $5K procedure and hundreds of patients a year that adds up to a lot of profit per clinic/physician.
I am not saying that they all are making no profit, but the idea that all of these doctors and clinics are raking in big bucks is not likely. First of all, many do not have hundreds of patients that they are treating yearly. Clinics devoted entirely to stem cell therapy may have hundreds of patients I suppose, but not individual doctors running small clinics.
Many doctors pay a fee for kits they use for adipose therapy. That takes a chunk out right up front. There is also insurance, employee salaries, taxes, rent, utilities, costs associated with any studies they may be doing, and all the other things that go with running a business. It all adds up. Unless one has owned their own business, there is usually a tendency to underestimate the costs of doing business.
One person I spoke with works for a publicly traded company. Most of their money has been put right back into the business to help fund their research and studies that they are conducting. No one there is making big bucks from stem cell treatments. The company exec I spoke with was incensed that anyone would think that and pointed out that it was a matter of public record.
I am not sure how you have arrived at the conclusion that most patients receive at least 3 procedures either. My last treatment was done under an IRB study that lasted a year. I was given one treatment. The doctor limited the number of participants and did follow up. He also said after the study that I could have an additional treatment at no cost if I wanted. I haven’t felt the need. He certainly didn’t get rich off of the study he conducted. I’m the one who hit the jackpot as I have had a lot of quality of life improvements.
I think there is just too much speculating going on. I know you would not conduct scientific research in such a manner. That’s why I am surprised when these assumptions are just put out there like there are verifiable financials to back them up.
If the clinics were more transparent about their fees and profits that would help bring more clarity to this question. To my knowledge such data has not been published in papers either. As a result, we have to go on what we have. Call me a skeptic, but if these docs weren’t making good money doing this, then I have to ask: why are they bothering to do it? Solely to help their patients? Hmm, I doubt it. Otherwise why do try to make any profit at all?
You also are critical of me for “speculating” based on my talking to people in the industry, but then you say “One person I spoke with…”, which seems to be exactly the same thing.
The bottom line –that I’m guessing we can both agree upon–is that having more concrete information in the public domain on all of this would be helpful to everyone. My impression is that the stem cell clinics are opposed to that.
I think there is a reluctance for doctors to advertise prices. If you are old enough to recall, I believe it used to be prohibited in fact. I would like to see prices advertised for all health services personally, not just stem cell treatments.
Also, I have knowledge of more than just one person that I spoke with. I mentioned that particular bit of information because it was a publicly traded company. You might try doing an interview sometime with a doctor or clinic owner and just ask them what costs are involved. I think it would be interesting for your readers. I don’t think anyone would fault them for making a decent living so I think you could get some to agree to discussing it.
So, today the FDA has banned “autologous fat stem cell therapies”. Tomorrow, will they be banning all the other types of autologous stem cell therapies (eg from bone marrow)?
Not banned, just regulated. Just like how regulating a drug through trials to ensure its safety and efficacy results in its safe and effective use (not banning).
The autologous model becomes economically infeasible if it is regulated on the same footing as a standardizable, mass-produced drug. Thus, it might be “regulation” in name but it is “ban” in fact.
As to your second point, drug-type regulation methodology does not ensure efficacy and safety. Look to the huge error made with statins for a blatant example.
I think that it is the observations of medical practitioners/patients and scientific measurements (the good-type science) that will show the extent to which a therapy is safe and the extent to which it is helpful for some condition.
To me, the regulatory approach taken by FDA seems reactive and contrived for the advantage of Big Pharma over medical practice.
I understand your point that bedside autologous cell transplantation may become economically infeasible for medical practitioners if regulated. However, the flip side of that is that if anyone, even those without an understanding of stem cell biology, can do it without any regulation of the process, cell quality, cell characteristics, etc, then what is to determine that any given treatment is safe or has efficacy? Are you suggesting that there is no variability among autologous cell preparations and no question as to their safety and efficacy?
Yes, errors have been made in drug regulation, and regulation may thus not guarantee safety. However, I think it is hard to argue that regulation does not increase safety. Consider that without regulation, not only those “error” drugs but also additional problematic drugs would also have been marketed. Also, without careful evaluation, the problems with the “error” drugs may not have even been discovered. Are you suggesting that overall, even taking the errors into account, the safety of drugs is not increased by regulation?
I think that the observations of medical practitioners/patients are important and useful, but they can also be anecdotal or shaped by biases, a desire to sell a service, or a desire to believe in an outcome. The “scientific measurements” and “good-type science” that you mention are derived from controlled trials.
The regulatory approach of the FDA does seem reactive given the timing, but I think that this is because of the recent increase in the popularity of such treatments. It is difficult for regulatory agencies to be proactive rather than reactive. I also don’t think that it is contrived for the benefit of Big Pharma; rather, I think that it is derived from a legitimate concern for patient safety and the actual efficacy of these treatments.
It is the notion that an individuals cells for an individuals treatment should be regulated as a “drug” that bothers me.
There are many types of regulation and many regulators — aside from that which you favour.
Looking back over my own life (as a patient), I’d say that knowledge is far more useful than regulation. Forty three years ago, I went along with “regulation and standard practice” — much to my misfortune. The funny thing was, there were publications, from 20 years previous, that clearly demonstrated the error that cost me so dearly. Only those publications were not accessible to a patient back then because there was no www.
I understand your point. I think that the question being raised, though, is that once you remove and manipulate the cells/tissue whether it can really be called your cells, i.e., your native cells, anymore, as changes may occur in the processing and then when they are re-implanted they are often being implanted into places they would not normally exist in nature or being asked to do things they would not normally be asked to do in nature.
As for other types of regulation and regulators, I agree that the FDA is not perfect, but I think it does improve the safety and consistency of therapeutics, and I am not sure what kind of other regulations or regulators would do a better job. Can you provide examples?
I also agree that knowledge is important and that if everyone had knowledge then perhaps regulations wouldn’t be as important. However, in this day and age, where many people believe everything they see on Google without critical analysis or evaluation, I think that is difficult for people to separate good information from bad information and obtain that knowledge. I believe that regulations are used to help protect people from making decisions based on faulty knowledge. Of course, as you mention, this assumes that regulations are based on the best available evidence at the time.
Brian, I think we can all agree that the FDA is imperfect in numerous ways as well as facing enormous challenges, however it seems like you are advocating an all or nothing kind of thing where if the FDA makes any mistakes we shouldn’t trust it all? I also did not say (I hope) that drug-type regulation ensures safety and safety, but it is hard to imagine that it doesn’t at least help improve the odds. What’s the alternative? To my knowledge, regulation of biologics such as manipulated stem cell products simply as 361s and HCT/Ps cannot improve safety or efficacy. All it can do is facilitate getting these products into patients more quickly. While that may be one of several goals that could have positive outcomes, in my mind the tradeoff of putting products into patients with less data backing up potential safety and efficacy is not worth it in the vast majority of cases with perhaps some very rare exceptions (e.g. expanded access/compassionate use for patients facing terminal illnesses).
As to the notion that Big Pharma controls the FDA and hence the FDA is anti-stem cells, that just doesn’t ring true at all to me.
No, Big Pharma does not control FDA. More that the business model makes them like symbionts. (Like us and bacteria in our guts — works in some ways, not in others.)
My view is that SVF is safe. However, one of the key aspects of these SVF clinics that is often overlooked is what does the SVF output look like? The answer is who the hell knows? Who knows how pure the output is and how many viable cells are present? This link illustrates the point by comparing four diferent SVF extraction systems: http://www.ncbi.nlm.nih.gov/pubmed/24281640. The results are very revealing. Its the wild wild west out there and buyers had better be aware of this before spending their money.
This is an excellent point, Ray, on the heterogeneity of the SVF products, devices, and such out there. What one clinic calls SVF may be wildly different than what another clinic calls it, etc.
I am not as convinced as you that SVF is by definition safe even if made in manner that is relatively consistent. There are risks including fibrosis, pulmonary emboli, abnormal tissue growth (e.g. bone in the face) and I’d say the risks increase when SVF is used in a systemic and/or non-homologous manner.
Paul, I agree with you that the FDA should clamp down here. I’d like know if you have any specific examples of issues related to a highly pure and scrutinized SVF output. The thing is that, the only company that has FDA 501k approval for this is Cytori Therapeutics and that would be your gold standard as indicated in the study I linked to in my comment. I don’t think you will find any safety concerns related to their output that they refer to as ADRCs. But I like to hear any other examples of problems with less than the gold standard that you mention.
Ray, your comments are interesting, and I agree that Cytori’s Celution system has shown promise (as a disclaimer, I co-authored on ASCs/MSCs with the founder of Cytori a long time ago). However, I was under the impression that Cytori only has 510(k) clearance for their fat contouring/fat grafting device, and that their stem cell devices were actually denied 510(k) and that the appeal was also denied about a year and a half ago. Has something changed more recently? If someone were to get 510(k) clearance for a stem cell transplantation system, I think it would be a really big deal.
Shisakin, you are correct. I was thinking Puregraft which they have divested. However they by have previously sold their equipment for “research” purposes in thre U.S. and the do have a CE Mark and approval in other countries. The pulled back on US commercial activity to stay in good graces with the FDA. They will benefit tremendously if they can get their act together.
Ray, that’s what I thought. Yes, I remember following their initial clinical trials in Japan and Germany 10 years ago. Exciting stuff.