How much does stem cell therapy cost in 2024? How have prices changed?
To authoritatively answer these questions now we need data from the present and past along with expert perspectives.
Some surprises come up in this new analysis.

In this article
Intro | Stem Cell Therapy Cost: $10,000-$20,000 | Why do stem cells cost so much? | Price changes | Cost of different treatments | Stem cell supplement cost | Does insurance or Medicare cover stem cell therapy? | Will stem cell therapy costs go down? | References
Fortunately, I have new polling data from mid-2023 so the stem cell cost numbers are up-to-date. I also polled on the number of stem cell treatments received.
The new data are notable for several reasons.
Let’s get started.
Intro on stem cell therapy cost
This post is the most comprehensive look at stem cell therapy cost and costs of related therapies that I’ve seen on the web, especially factoring in our inclusion of historical polling data from past years here on The Niche.
You can also watch the video above where I summarized the key points about stem cell cost.
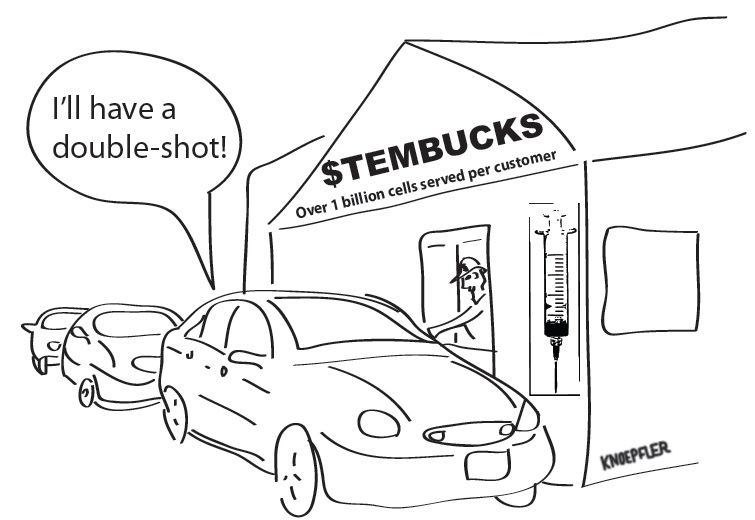
Today’s post also goes over other important issues related to insurance, fundraising, and approaches to being a smart consumer. Keep in mind that almost all stem cell “therapies” outside the bone marrow/hematopoietic sphere are not FDA-approved. Those interventions mostly lack rigorous data to back them up too. So this post is not recommending you get them. I advise against going in that direction, but many people still want info on cost.
After more than a decade of blogging about stem cells from just about every angle and doing research myself in my lab here at UC Davis School of Medicine, it’s interesting to consider trends in the types of questions I get asked. Beyond cost, I also often get asked How much of a stem cell treatment price does insurance cover?
Of course, insurance (or lack thereof) directly bears on stem cell therapy cost too. I’ll get more into insurance later in the post.
Polling data on stem cell therapy cost: $10,000 to $20,000
In 2023, the most selected price is $10,000-$20,000 for a stem cell therapy. The price range of $2,501-$5,000 was the second-most-picked answer.
A sizable fraction of people paid between $20,000 and $100,000, which is very expensive.
What about the number of injections?
The most common answer for the number of stem cell injections is one. It’s still remarkable that a substantial population of people get numerous injections. Almost one in ten people have gotten more than 10 stem cell therapies.
While this kind of polling isn’t perfect it can gauge trends. Unfortunately, I haven’t seen much other published data on stem cell clinic offering costs in actual journals.

Why do stem cell injections cost so much?
Why is this so expensive?
To have a sense of cost, we need to ask patients certain questions. How much did you pay per injection? How many injections did you get? Where did you get them?
Keep in mind that the total cost of stem cell “therapy” is the product of the cost per injection times the # of injections. For instance, if a stem cell injection costs $8,000 and you get 10 injections, your total cost is $80,000. On the other hand, even one $100,000 stem cell therapy can have a major negative impact on someone’s finances. People often turn to family, friends, and online fundraising like GoFundMe.
Unfortunately, the unproven stem cell clinics generally do not volunteer data on how much they charge. They also often encourage patients to get many injections.
All of this can run up the total cost.

Data on price changes for stem cell shots
Compared to me historical data, prices may have gone up at most just a little for stem cells. I thought there would be more of a jump so this is surprising.
Our 2020 polling data also had “$10,001-$20,000” as the most common answer, the same as 2023, while $2,501-$5,000 was the second most selected answer in both cases.
While the most common answer on stem cell therapy cost in 2019 was $2,501-$5,000 so prices are much higher now versus 2019. For comparison, the full 2019 polling can be found here.
What you can see from 2019 is that a plurality of respondents reported getting one stem cell injection, but 60% of people nonetheless got more than one stem cell injection.
Stem cell cost for different kinds of treatments
Stem cell therapy costs can vary substantially depending on the type. Below I’ve listed the best available stem cell treatment cost by type in the U.S.
- Cost of stem cell therapy for knees. The average cost of stem cell shots for knees is lower than most other procedures. It typically ranges between $5,000-$10,000.
- Cost of stem cell therapy for back pain and shoulders. Cost ranges between $5,000-$15,000. Injections into discs can be trickier.
- Cost of stem cell treatment for neuropathy. While I have seen price tags of $2,500-$5,000 here, the upper end of cost has been going up into the tens of thousands of dollars.
- Cost of stem cell therapy for vision loss. These procedures start around $20,000 and go higher. Based on adverse events including loss of vision, these are also some of the riskiest procedures out there. There just aren’t data to support these offerings.
- Cost of stem cell therapy for autism. There is no proven safe and effective stem cell therapy for autism, but various offerings are still available. At Duke the cost for getting unproven cord cells has been around $15,000 but they are no longer offering it at the moment. Outside the U.S. the price for cord cells for autism is generally $20,000 and up. Note that the cells used are often not actual stem cells.
- Stem cell cost for bone marrow transplantation. Bone marrow or hematopoietic stem cell transplantation are very different matters than the others listed here. The cost can be $100,000-$200,000 or even higher, but this is generally covered by insurance for standard procedures such as treating blood cancers.
Stem cell treatment cost also varies based on location but we’ve seen some movement toward similar prices inside versus outside the U.S. Interestingly, if anything, prices are generally higher outside the U.S. now such as in Mexico, Colombia, and Panama.
The prices there are generally not lower than $20,000.
Stem cell supplement costs including Regenokine
There is growing interest from the public in stem cell supplements. I did a post on this earlier in 2023 so take a look here, which was essentially a review of stem cell supplements like Regenokine. In terms of cost, while supplements are far less expensive than getting stem cell, PRP, or exosome injections, supplements are still pricey for what you get.
It’s not unusual to pay $100 for a small bottle of stem cell supplements, the other factor to consider is that these supplements generally have no solid, published data behind them so you might as well be paying $100 for water. It’s unclear what risks taking these supplements might bring as well.
Does insurance or Medicare cover stem cell therapy?
A common question I hear is the following: is stem cell therapy covered by insurance? Unfortunately for patients desperate to try stem cells, insurance generally does not provide any coverage, which often leads them to take extreme financial measures. These steps can include fundraising (more below).
In my view, the Regenexx brand has made a big deal out of how some employers contribute towards costs of their clinics’ offerings. I’m not so clear on where that stands today in 2023
Does Medicare cover stem cell therapies? Medicare will generally cover the cost of established bone marrow transplantation-type therapies. However, Medicare does not cover unproven stem cell “therapies.”
Looking ahead will stem cell therapy costs go down?
There is pressure on stem cell clinics now in 2023 in large part due to two factors. These could drive costs down or up depending on how things play out. First, the FDA is more active against unproven stem cell clinics. This may mean more money from the clinics going toward paying attorneys or FDA compliance experts. You’d think this might drive costs up. However, the still large number of clinics may keep pressure to not raise price tags.
To sum up, the answer to the question, “How do stem cells cost?” largely depends on context. Overall, clinics will charge what they think patients will pay them. It will always be a moving target.
I urge patients to be cautious both medically, talking to their doctors, and financially.
References on stem cell therapy cost
- The Trouble With Stem Cell Therapy, Jeneen Interlandi, Consumer Reports, January 11, 2018.
- FTC Returns Almost $515,000 to Consumers Who Bought Deceptively Marketed “Amniotic Stem Cell Therapy” Between 2014 and 2017, Federal Trade Commission, April 30, 2019.
- Crowdfunding, stem cell interventions and autism spectrum disorder: comparing campaigns related to an international “stem cell clinic” and US academic medical center. Cytotherapy. 2020 Oct 17:S1465-3249(20)30857-4. doi: 10.1016/j.jcyt.2020.09.002.
My spine filled with blood during a spine cord stimulator trial for sciatica. One of the leads poked thru around the t8 and blood entered and pooled around the t3 where I had a previous putty fusion surgery. Paraplegic for 6 months then some movement in one leg started the learning to walk again therapy. A blood clot in my foot broke up in one leg stopping my progress. Leaving me with absurd chronic pain and partially paralyzed in that leg, it’s been 8 years now and worsened with age (I’m 63). Would I be a candidate for overseas stem cell treatment?
mine is quoted at roughly 20000 usd for 30 mill stem cells dirved from human placenta, non -frozen, 2023
Where was this at?
Keep in mind that many of the testimonials for these ‘treatments’ are paid clients, either receiving discounts or free product. And they NDA’s to prevent them from talking about negative adverse events.